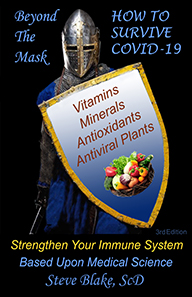
Beyond the Mask
How to Survive COVID-19
Strengthen Your Immune System
4th Edition
Steve Blake, ScD
March, 2021
I have searched the scientific medical journals so that I can explain
why so many people get no symptoms when exposed to COVID-19.
The human immune system can kill off invading viruses
effectively if it has the necessary nutrients.
Many of these nutrients needed by the immune system are
essential vitamins and minerals.
These nutrients are also needed for a good responce to vaccination.
The science is clear that two of these nutrients stand out as being
crucial in correcting the decline of the immune system in old age.
I can show you which compounds in safe foods fight the virus inside our bodies.
We can stop attachment of COVID-19 to our cells and reduce its replication.
We can reduce the excess inflammation that can lead to a cytokine storm.
I will also outline the most effective medical plants for resisting viruses
based upon peer-reviewed science. We need to do more than wear masks.
Now is the time to boost our immune systems and boost our health!
$10 to download the entire 126 page ebook
Click Below:
$25 to download the entire 126 page ebook.
Thank you for the extra suport!
Click Below:
Table of Contents
What you will learn to protect yourself: - 2
Introduction - 5
Table of Contents - 8
Who is most at risk from COVID-19 - 12
Obesity and Covid-19 - 14
Making vaccines work better - 18
Inflammation and COVID-19 - 23
Cytokine storm - 23
Reduce inflammation with PPAR-gamma - 26
Omega-3 fatty acids - 27
Resveratrol from red grapes - 27
Curcumin from turmeric - 28
Thyme and Oregano - 29
Rosemary and sage - 30
Hot peppers - 30
Pomegranate - 31
Lemongrass - 31
Kale, cabbage, and broccoli - 32
Astaxanthin - 33
Inflammation and blood clotting - 33
Endotoxins increase inflammation - 34
Advanced glycation endproducts - 35
Arachidonic acid - 35
Multivitamins - 37
Micronutrients for immune power - 37
Vitamin forms and amounts - 38
Antioxidants - 39
Vitamin and mineral deficiencies in elders - 42
Brain and Body Food - 44
Vitamins and Minerals - 46
Vitamin A - 46
Vitamin D - 46
Vitamin B12 - 49
Folate - 50
Vitamin C - 51
Vitamin E - 52
Vitamin E and antioxidant activity - 53
Vitamin E and ageing - 55
Vitamin E and immune response - 56
Vitamin E helps with inflammation - 58
Vitamin E, pneumonia, and bacterial infections - 59
Vitamin B6 - 60
Selenium - 61
Zinc and viral infections - 62
Zinc in ageing - 63
Zinc and acute respiratory distress - 66
Food and spices as powerful as antiviral drugs - 68
Slowing virus attachment to our cells - 68
Sweet cherries and bitter orange - 68
Green tea, turmeric, parsley, and oats - 69
Lectins, leeks and nettles - 71
Food, drinks, and spices to stop COVID-19 - 72
Licorice and glycerrhizin - 72
Baicalin and skullcap - 73
Quercetin and luteolin - 74
Skullcap, rosemary, and hispiduline - 75
Grapes and resveratrol - 76
Slowing virus replication with food and spices - 77
Vitamin B2 - 77
Figure 3 Food nutrients to slow COVID-19 viral replication. - 78
Artichoke, turmeric, parsley, and green tea - 79
A meal to slow virus replication - 79
Skullcap and scutellarein - 80
A meal to inhibit COVID-19 - 80
Quercetin - 81
Indian plants to slow replication - 82
Myricetin from healthy food - 83
Naringin - 84
Hesperidin - 84
Glutathione, vitamins B1 and E, and biotin to inhibit COVID-19 - 85
Medical plants to boost immune power - 87
Echinacea - 87
Maitake and Reishi mushrooms - 88
Cranberry and soy isoflavones - 89
Black Cumin - 90
Ginseng - 92
Goldenseal - 93
Astragalus - 94
Turmeric - 95
Garlic - 97
Chinese herbal medicine formula qingfei paidu tang - 98
Chinese herbal medicine formula Lianhuaqingwen - 99
References to scientific studies - 114
INDEX
3C-like protease, 80
ACE2
and vitamin D, 48
attachment reduced by hispidulin, 75
increased expression, 74
inhibited by baicalin, 73
resveratrol reduces binding, 76
ACE2 receptor, 68
inhibitors, 68
acute respiratory distress
and antioxidants, 41
acute respiratory distress syndrome, 23
and vitamin E, 53
acute respiratory tract infection
and vitamin D, 49
adaptive immune system, 25
and vitamin D, 48
advanced glycation endproducts, 35
age and COVID, 12
age-associated decline in natural killer cells, 56
age-associated immune loss
and vitamin E, 55
aged cheese, 35
ageing immune system
and vitamin E, 52
agglutinin lectin, 71
ajoene
and garlic, 97
allicin
and garlic, 97
almonds, 66
aloe vera
reduced binding, 83
alpha lipoic acid, 86
alpha-hederin
and black cumin, 91
Alzheimer's disease, 35
analgesic, 31
angiotensin converting enzyme-2. See ACE2 receptor
animal fat
and arachidonic acid, 35
anthocyanins
in cranberry, 89
antibodies
4 to 7 days for specific antibodies, 25
improved with multivitamins, 43
vItamins C, E, and zinc, 43
antibody defenses, 68
antibody production
and garlic, 97
impaired with low vitamin E, 57
antibody response
and turmeric, 95
improved with zinc, 63
antigen stimulation
enhanced by selenium, 61
anti-inflammatory, 26, 29, 31
and vitamin E, 55
cayenne, 30
lemongrass, 31
antimicrobial
and garlic, 97
goldenseal, 93
antioxidant, 29, 31
and turmeric, 96
baicalin, 73
antioxidant enzymes, 27, 40
antioxidants, 39, 85
and immune cells, 39
resistance and recovery, 41
anti-viral
and vitamin C, 51
glycyrrhizin, 73
oats, 70
scutellarein, 80
anti-viral defenses, 24
apigenin
COVID-19 replication inhibitor, 79
inhibits ACE2, 70
more powerful than an antiviral drug, 70
apoptosis, 64
arachidonic acid, 35, 87
and vitamin E, 59
arteries
adhesion problems, 28
artichoke
COVID-19 replication inhibitor, 79
ashwagandha
reduced binding, 83
astaxanthin, 33
astragalus, 94
attachment of the COVID-19 virus
inhibited by glycyrrhizin, 72
B- and T-cell-mediated immune responses
ginseng, 92
baicalin, 73
twice as powerful as an antiviral drug, 74
barbequing
and advanced glycation endproducts, 35
barberry
inhibit ACE2, 69
B-cells
and astragalus, 94
and turmeric, 95
losses without zinc, 63
berberine
and pneumonia, 94
beta- sitosterol, 99
beta-D-glucan, 88
beta-glucan
inhibit ACE2, 70
inhibits ACE2 for a day, 70
biotin
inhibit viral growth, 85
bitter orange
inhibit ACE2, 69
black cumin
inhibits docking of COVID-19, 91
black cumin oil, 90
black pepper, 28
black rice, 66
black sesame, 66
Brain and Body Food, 44
Brazil nuts
may be radioactive, 62
bronchodilating
and black cumin, 90
calcitriol
and inflammation, 48
capsaicin, 30
cardiovascular disease
and risk, 12
carnosic acid, 30
carnosol, 30
carotenoids, 40
carvacrol, 29
catechin
COVID-19 replication inhibitor, 79
cayenne, 30
celery, 66
cell-mediated immunity
improved by vitamin B6, 61
cellular immune response
enhanced by selenium, 61
chemokines, 24, 25, 61
and turmeric, 95
chicken
and arachidonic acid, 35
Chinese herbal medicine, 98
chloroquine, 83, 91
chocolate, 40
chronic diseases
and risk, 13
citral, 31
citrus
reduce binding to ACE2, 76
citrus fruits, 84
clotting, 34
coagulation
excess, 34
comorbidities in Covid, 13
copper, 21, 38
copper, zinc, and manganese, 40
coronavirus spike glycoprotein
lectins inhibit COVID-19, 71
COVID-19
attachment and vitamin D, 48
inhibited by Chinese formula, 98
COVID-19 inhibitory effect
baicalin, 73
COVID-19 main protease, 85
COVID-19 proteases
inhibited by hesperidin, 84
COVID-19 replication
lianhuaqingwen, 99
COX-2, 27, 29, 30
and lemongrass, 32
and vitamin E, 59
cranberry, 89
C-reactive protein, 33
curcumin, 28, 81
better than hydroxychloroquine, 75
COVID-19 replication inhibitor, 79
inhibits ACE2, 70
inhibits replication, 96
cyclooxygenase
and echinacea, 87
cyclooxygenase-2. See COX-2
cytokine, 24
cytokine storm, 23, 25, 26, 28, 33
and advanced glycation endproducts, 35
and arachidonic acid, 36
and PPAR-gamma, 28
and turmeric, 95
and vitamin D, 48
in COVID-19, 32
cytokines, 23, 27, 31, 33, 48
and astragalus, 94
and ginseng, 92
and lemongrass, 31
and turmeric, 95
and vitamin D, 47
inhibit pro-inflammatory, 26
lianhuaqingwen, 99
which are elevated in cytokine storm, 25
dementia
how to reduce, 13
dendritic cells
and beta-D-glucan, 89
and turmeric, 95
diabetes
and risk, 12
echinacea, 87
eggs
and arachidonic acid, 35
elderly
improving antibody recognition, 43
nutritional deficiency is common, 21
elders
and folate, 50
and vitamin D deficiency, 47
and zinc, 64
deficient in zinc, vitamins A E & D, 43
low zinc. selenium, and vitamin C, 42
produce interferon like youths with zinc, 65
elders 85 and older
are 32 times more likely to die of influenza, 47
elders are susceptible to zinc deficiency, 65
endotoxins, 34
and cytokine storm, 34
not in plants, 34
epigallocatechin gallate, 69
fat-soluble antioxidants, 40
favipiravir, 91
fever, 28, 36, 60, 87
and black cumin, 90
fiber
reduces respiratory infections, 40
fibrinogen, 34
fisetin, 84
fish, 35
fish oil
polluted and rancid, 27
flavone glucuronide, 73
folate, 50
free radical damage, 39
fruits and vegetables
boosted vaccine response, 20
garlic, 81, 97
inhibit ACE2, 69
ginger
reduced binding, 83
ginseng, 92
ginsenosides, 92
glutathione, 85
and turmeric, 96
best inhibitor of main protease, 85
glutathione peroxidase, 40
glycyrrhizin, 72
goldenseal, 93
grapefruit
disrupts replication of COVID-19, 84
grapes
reduce binding to ACE2, 76
green tea, 69
COVID-19 replication inhibitor, 79
duration of virus inhibition, 69
Guduchi
reduced binding, 83
hesperidin, 84
high blood pressure
and risk, 12
hispidulin, 75
humoral immunity
improved by vitamin B6, 61
hydroxychloroquine, 75, 82, 83, 91
immune cell function
enhanced by garlic, 98
immune cells
and vitamin E, 54
immune defense
30-80% loss with low zinc, 63
improved by vitamin B6, 60
improved with zinc supplementation, 63
immune function
and folate, 50
improved by vitamin B6, 60
increased vitamin/mineral, 42
immune response
and obesity, 14
in the elderly, 18
raised by vitamin E, 56
immune stimulation
and vitamin C, 51
immune system
and ageing, 43
immune system stimulators, 88
immunity
to COVID-19, 77
immunoglobulin A antibodies
and goldenseal, 93
infected cells
selenium helps kill them, 61
infection
and vitamin A, 46
infections
folate is protective, 50
infections in institutionalized patients
reduced by half, 42
inflammation, 23, 27, 30
and advanced glycation endproducts, 35
and arachidonic acid, 35
and astragalus, 94
and black cumin, 90
and COX-2, 27
and curcumin, 28
and echinacea, 87
and ginseng, 92
and multivitamin/mineral, 23
and vitamin D, 48
and vitamin E, 59
and zinc, 65
astaxanthin, 33
excessive, 33
from endotoxins, 34
in cytokine storm, 25
reduced by selenium, 61
inflammatory cascade, 27
inflammatory cytokines, 25
improved with vitamin E, 58
inflammatory prostaglandin
decreased by vitamin E, 56
inflammatory reactions
and echinacea, 87
inflammatory response, 24
influenza
reducing incidence, 44
inhibit the replication of COVID-19
quercetin, 81
inhibiting virus replication
lianhuaqingwen, 99
inhibitor of covid-19's main protease
quercetin and curcumin, 81
innate immune system, 23
and vitamin C, 52
innate immunity
and vitamin D, 46
improved with zinc, 63
interferon, 24, 65
and astragalus, 95
and echinacea, 87
and vitamin C, 51
and zinc, 65
stimulated by glycyrrhizin, 72
interferon gamma, 15
interferon-gamma, 25, 59
and ginseng, 92, 93
interleukin, 24
and ginseng, 92
interleukin-1 and 2
and reishi, 89
interleukin-12, 89
interleukin-2, 25
interleukin-6, 33
and astragalus, 94
lianhuaqingwen, 99
interleukin-7, 25
iodine, 21
iron, 21
kaempferol, 99
lectins, 71
Leeks
inhibit attachment of COVID-19, 71
legumes, 66
lemongrass, 31
lentils, 66
leptins, 14
leucocytes, 39
leukotrienes, 27, 29, 30, 32, 87
and arachidonic acid, 35
and vitamin E, 59
lianhuaqingwen, 99
licorice, 72
lipopolysaccharides, 34
liposomal reduced glutathione, 86
lipoxygenase
and echinacea, 87
lung damage
and vitamin C, 51
lung disease
more severe without selenium, 61
lung inflammation, 34
and ginseng, 92
lung-cleaning and toxicity-excluding soup, 98
lungs
and lungs in COVID-19, 23
small vessel damage, 42
vitamin A protects, 46
luteolin, 84, 99
COVID-19 replication inhibitor, 79
lowers ACE2, 74
lymphocyte counts
improved with zinc, 63
lymphocyte functions
improved with zinc, 63
lymphocyte proliferation
and vitamin C, 52
improved by vitamin B6, 60
lymphocyte responses, 43
lymphocytes
and ginseng, 92
lymphokines, 24
and echinacea, 87
and garlic, 97
macrophage
and goldenseal, 93
macrophages, 43, 89
and astragalus, 94
and garlic, 97
and turmeric, 95
and vitamin A, 46
need zinc, 63
main protease of COVID-19, 82
maitake, 88
malondialdehyde, 41
meat, 35
membrane phospholipids, 53
Memory T cells
and obesity, 14
micronutrients, 37
in immune functioning, 19
minerals
supplementry amounts, 38
to reduce risk, 37
monocytes, 43
mucous membranes
and goldenseal, 93
and vitamin A, 46
multivitamin/mineral supplementation, 41
multivitamin/mineral supplements, 42
doubled antibodies in children, 44
multivitamins
and white blood cells, 43
improved natural killer cells, 43
mushroom, 66
mushrooms, 88
myricetin, 83
myricetin sources, 84
N-acetyl cystein, 86
naringin, 84
disrupts replication of COVID-19, 84
natural killer cell activity
and vitamin C, 51
natural killer cells, 43
ageing and folate, 50
and echinacea, 87
and garlic, 97
and ginseng, 93
and maitake, 89
and turmeric, 95
and vitamin A, 46
improved by vitamin B6, 60
improved with vitamin E, 57
improved with zinc, 64
neem
reduced binding, 83
Nelfinavir, 70, 81, 84, 85
neuraminidase
and turmeric, 96
neutrophils
and turmeric, 95
and vitamin A, 46
improved with vitamin E, 57
need zinc, 63
nigelledine, 91
nigellone
in black cumin, 90
nuclear factor kappa-B, 27, 30
nutritional supplement, 22
nuts, 66
oats
inhibits ACE2, 70
obesity
and Covid-19, 14
and increased risk of severe Covid-19, 15
severe obesity and Covid-19, 17
omega-3 fatty acids, 27
onions, 81
oregano, 29
Oxford vaccine
and elderly antibody levels, 18
oxidation
and vitamin E, 54
oxidative stress, 39
and vitamin E, 53
pain, 28, 60, 87
papain-like protease, 80
parsley
COVID-19 replication inhibitor, 79
peroxisome proliferator receptor-gamma. See PPAR-gamma
phagocytic activity
and vitamin C, 51
phagocytosis
and garlic, 97
less without zinc, 63
phospholipase, 59
phospholipids, 53
pneumonia, 23
and echinacea, 88
and goldenseal, 94
and vitamin C, 52
and vitamin E, 59
reduced prevalence with zinc, 66
zinc reduces risk and duration, 64
polyphenols, 40
polysaccharides, 88
and echinacea, 87
pomegranate, 31
poultry, 35
PPAR-gamma, 26, 30
and lemongrass, 31
pomegranate, 31
prevent cytokine storm, 32
rosemary and sage, 30
thyme and oregano, 30
pro-inflammatory cytokines, 61
prostaglandin
and vitamin E, 60
prostaglandins, 36, 87
pumpkin seeds, 66
punicic acid, 31
anti-inflammatory from pomegranate, 31
qingfei paidu tang, 98
quercetin, 75, 81
in Chinese formula, 99
low toxicicty, 81
lowers ACE2, 74
reduces COVID-19 proteins, 74
stops attachment of COVID-19 to cells, 75
reactive oxygen species
from inflammatory reactions, 27
recovery time
reduced with astaxanthin, 33
red onion
reduced binding, 83
reishi, 88
remdesivir, 77
replication
hispidulin blocks main protease, 75
replication inhibition
scutellarein, 81
replication of COVID-19
and vitamin D, 48
myricetin slows replication, 83
research studies, 45
resistance to infection
and vitamin E, 55
respiration
improved with zinc, 63
respiratory infections from influenza
lowered by vitamin E, 56
resveratrol, 27, 76
RNA polymerase, 77
rosemary, 30, 75
hispidulin, 75
rutin
reduces binding of COVID-19, 76
sage, 30
SARS, 47
Scutellarein, 80
Scutellaria baicalensis, 73
selenium, 19, 40, 61
and cure rate from Covid-19, 19
and vaccination, 20
sources, 62
selenium deficiency
in the elderly, 21
sesquiterpenes
in echinacea, 87
severe acute respiratory syndrome
inhibited by zinc, 66
severe lung disease
and inflammation, 26
skullcap, 73, 80
can inhibit replication of COVID-19, 73
hispidulin, 75
sedative effects, 74
soy, 66
soy isoflavone, 90
spike protein
resveratrol disrupts binding to ACE2, 76
Steve Blake website, 12
stigmasterol, 98
stilbene, 76
stinging nettles
lectins inhibit COVID-19, 71
strokes, 13
sunflower seeds, 66
superoxide dismutase, 38, 40
and astragalus, 95
supplementation, 37
supplements
and SOD, 41
susceptibility to influenza infection, 62
sweet cherries
inhibit ACE2, 68
T- and B-lymphocytes
and garlic, 97
Tamiflu, 90
T-cell activity
and vitamin C, 51
T-cell proliferation
and vitamin E, 56
T-cells
and beta-D-glucan, 89
and ginseng, 93
and turmeric, 95
enhanced by selenium, 61
improved by vitamin B6, 60, 61
improved with vitamin E, 57
losses without zinc, 63
tea, 40
T-helper cells, 43
thiamin
inhibits COVID-19, 85
thyme, 29
thymochinone
in black cumin, 90
T-lymphocytes
and echinacea, 87
improved with zinc, 64
in ageing, 63
tolerable upper limit
for copper, 39
toll-like receptor
and astragalus, 95
and ginseng, 92
trace elements, 21
trace minerals, 41
tumor necrosis factor, 25, 30
and astragalus, 94
and zinc, 65
tumor necrosis factor-alpha, 25, 99
and ginseng, 92
turkey
and arachidonic acid, 35
turmeric, 28, 95
COVID-19 replication inhibitor, 79
reduced binding, 83
uncontrolled viral replication, 47
upper respiratory infection
reduced with vitamin E, 58
vaccination
response, 15
vaccination responses
improved with vitamins and minerals, 20
vaccinations
and nutrients, 18
and obesity, 14
vaccine, 25
vaccine responses
and vitamins and minerals, 19
viral attachment
lectins inhibit COVID-19, 71
viral infection
and goldenseal, 94
viral infection of COVID-19
and vitamin B12, 49
viral infections
and glutathione, 85
and zinc, 65
reduced 1/3 to 2/3 with vitamins/minerals, 42
viral neuraminidase, 96
viral replication, 79
and thiamin, 85
and vitamin B12, 49
viral respiratory infections
and echinacea, 88
virus infections
dramatically reduced with zinc, 65
virus replication, 77
slowed 16 times, 90
virus-infected cells
zinc helps removal, 64
vitamin
minimum amounts, 38
vitamin A, 46
vitamin and mineral deficiencies, 42
vitamin B12, 49, 50
Vitamin B2
same power as remdesivir, 77
vitamin B6, 60
higher needs than RDA, 60
upper limit, 38
vitamin C, 51
and lungs, 93
sources, 40
vitamin D, 46
and cytokine storm, 25
deficiencies, 46
deficiency, 48
forms, 38
low levels greater risk, 47
more deaths in deficiency, 47
vitamin D supplementation
lowers viral replication, 47
vitamin D3, 38
vitamin E, 52
25 times less virus in lungs, 55
amount to boost immune response, 20
and free radicals, 54
boosted immune response, 20
deficiency, 40
deficiency 90 percent, 52
improves membrane integrity, 54
inhibits COVID-19, 85
made the immune system younger, 57
minimum versus needed amount, 52
most powerful antioxidant, 54
RDA, 52
tolerable upper level, 52
vitamin E sources, 40
vitamin E supplementation
increased T-cells, 55
vitamin E, at least 200 IU daily
raised immune response in elderly2-6 times, 56
vitamins, 37
vitamins and mineral
in vaccination response, 19
vitamins and minerals
are needed to be supplemented, 19
limit Covid vaccines, 21
needed for vaccination, 21
vitamins C and E, 39
white blood cells, 39
and astragalus, 94
whole plant foods
and antioxidants, 39
wogonin, 99
zinc, 19, 63
safe amounts, 39
upper daily limit, 65
zinc deficiency
about half of elderly, 21
common in elders, 64
zinc lozenges
and safety, 39
zinc sources, 66
References to scientific studies (147)
-
->Stock, James H., et al. "Estimates of the undetected rate among the sars-cov-2 infected using testing data from iceland." medRxiv (2020).
->Ioannidis, John PA, Cathrine Axfors, and Despina G. Contopoulos-Ioannidis."Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters." medRxiv (2020).
->Matsushita, Kunihiro, et al. "The relationship of COVID-19 severity with cardiovascular disease and its traditional risk factors: A systematic review and meta-analysis." medRxiv (2020).
->COVID-19 Surveillance Group. "Characteristics of COVID-19 patients dying in Italy: report based on available data on March 20th, 2020. Rome, Italy: Instituto Superiore Di Sanita; 2020."
->Pellini, Raul et al. “Obesity may hamper sars-cov-2 vaccine immunogenicity.” MedRxiv 2021.
->Zhang, Anna, et al. “Leptin Mediates the Pathogenesis of Severe 2009 Pandemic Influenza A(H1N1) Infection Associated With Cytokine Dysregulation in Mice With Diet-Induced Obesity.” The Journal of Infectious Diseases 2013; 207:1270–80.
->Karlsson, Erik, et al. “Diet-Induced Obesity Impairs the T Cell Memory Response to Influenza Virus Infection.” The Journal of Immunology, 2010, 184: 3127–3133.
->Jahn, Janine et al. “Decreased NK Cell Functions in Obesity can be Reactivated
by Fat Mass Reduction.” Obesity (2015) 23, 2233-2241.
->Popkin, Barry et al. “Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships.” Obesity Reviews. 2020;1–17.
->Richardson, Safiya et al. “Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area.” JAMA.2020;323(20):2052-2059.
->Caussy, Cyrielle et al. “Prevalence of obesity among adult inpatients with COVID-19 in France.” Lancet diabetes-endocrinology Vol 8 July 2020.
->Gau, Feng et al. “Obesity Is a Risk Factor for Greater COVID-19 Severity.” 2020, Diabetes Care.
->Kalligeros, Markos, et al. "Association of obesity with disease severity among patients with coronavirus disease 2019." Obesity 28.7 (2020): 1200-1204.
->Simonnet, Arthur et al. “High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation.” Obesity (2020) 28, 1195-1199.
->Rayman, Margaret and Calder “Optimising COVID-19 vaccine efficacy by ensuring nutritional adequacy” 2021, British Journal of Nutrition doi:10.1017/S0007114521000386.
->Ramasamy MN et al. (2021) Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomized, controlled phase 2/3 trial. Lancet 396, 1979–1993.
->Calder, Philip et al. “Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections.” Nutrients 2020, 12, 1181.
->Gombart, Adrian F., Adeline Pierre, and Silvia Maggini. "A review of micronutrients and the immune system–working in harmony to reduce the risk of infection." Nutrients 12.1 (2020): 236.
->Zhang, Jinsong, et al. "Association between regional selenium status and reported outcome of COVID-19 cases in China." The American journal of clinical nutrition 111.6 (2020): 1297-1299.
->Gibson, Andrew et al. “Effect of fruit and vegetable consumption on immune function in older people: a randomized controlled trial.” American Journal of Clinical Nutrition 2012;96:1429–36.
->Meydani, Simin Nikbin, et al. "Vitamin E supplementation and in vivo immune response in healthy elderly subjects: a randomized controlled trial." Jama 277.17 (1997): 1380-1386.
->Broome CS, McArdle F, Kyle JAM, et al. (2004) An increase in selenium intake improves immune function and poliovirus handling in adults with marginal selenium status. American Journal of Clinical Nutrition 80, 154–162.
->Vural Z, Avery A, Kalogiros DI, et al. (2020) Trace mineral intake and deficiencies in older adults living in the community and institutions: a systematic review. Nutrients 12, 107.
->Richardson, David et al. “Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective.” British Journal of Nutrition (2021), 125, 678–684.
->Rayman, Margaret and Calder “Optimising COVID-19 vaccine efficacy by ensuring nutritional adequacy” 2021, British Journal of Nutrition doi:10.1017/S0007114521000386.
->Mikirova, N., et al. "Effects of micronutrient supplementation on concentrations of vitamins and minerals, inflammation and cardiovascular risk factors." Vitam Miner 3.120 (2014): 2.
->Wang, Y.;Wang, Y.; Chen, Y.; Qin, Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J. Med. Virol. 2020, 92, 568–576.
->Mehta, Puja, et al. "COVID-19: consider cytokine storm syndromes and immunosuppression." The Lancet 395.10229 (2020): 1033-1034.
->Daneshkhah, Ali, et al. "The Role of Vitamin D in Suppressing Cytokine Storm in COVID-19 Patients and Associated Mortality." medRxiv (2020).
->Ciavarella, Carmen, et al. "Pharmacological (or Synthetic) and Nutritional Agonists of PPAR-γ as Candidates for Cytokine Storm Modulation in COVID-19 Disease." Molecules 25.9 (2020): 2076.
->Fats and Oils Demystified, A Guide to their Health Effects, Steve Blake, 2017, LifeLong Press. https://drsteveblake.com/fats-and-oils.html.
->Yao, Q.; Liu, J.; Zhang, Z.; Li, F.; Zhang, C.; Lai, B.; Xiao, L.; Wang, N. Peroxisome proliferator-activated receptor->(PPAR) induces the gene expression of integrin V5 to promote macrophage M2 polarization. J. Biol. Chem. 2018, 293, 16572–16582.
->Nakata, Rieko, et al. "Evaluation of Food-derived Functional Ingredients According to Activation of PPAR and Suppression of COX-2 Expression." Food Science and Technology Research 19.3 (2013): 339-345.
->Ciavarella, Carmen, et al. "Pharmacological (or Synthetic) and Nutritional Agonists of PPAR-γ as Candidates for Cytokine Storm Modulation in COVID-19 Disease." Molecules 25.9 (2020): 2076.
->Suntres, Z.E.; Coccimiglio, J.; Alipour, M. The bioactivity and toxicological actions of carvacrol. Crit. Rev. Food Sci. Nutr. 2015, 55, 304–318.
->Ciavarella, Carmen, et al. "Pharmacological (or Synthetic) and Nutritional Agonists of PPAR-γ as Candidates for Cytokine Storm Modulation in COVID-19 Disease." Molecules 25.9 (2020): 2076.
->Rau, O.;Wurglics, M.; Paulke, A.; Zitzkowski, J.; Meindl, N.; Bock, A.; Dingermann, T.; Abdel-Tawab, M.; Schubert-Zsilavecz, M. Carnosic acid and carnosol, phenolic diterpene compounds of the labiate herbs rosemary and sage, are activators of the human peroxisome proliferator-activated receptor gamma. Planta Med. 2006, 72, 881–887.
->Park, J.-Y.; Kawada, T.; Han, I.-S.; Kim, B.-S.; Goto, T.; Takahashi, N.; Fushiki, T.; Kurata, T.; Yu, R. Capsaicin inhibits the production of tumor necrosis factor alpha by LPS-stimulated murine macrophages, RAW264.7:A PPAR gamma ligand-like action as a novel mechanism. FEBS Lett. 2004, 572, 266–270.
->Ciavarella, Carmen, et al. "Pharmacological (or Synthetic) and Nutritional Agonists of PPAR-γ as Candidates for Cytokine Storm Modulation in COVID-19 Disease." Molecules 25.9 (2020): 2076.
->Nakata, R.; Takizawa, Y.; Takai, A.; Inoue, H. Evaluation of Food-derived Functional Ingredients According to Activation of PPAR and Suppression of COX-2 Expression. Food Sci. Technol. Res. 2013, 19, 339–345.
->Ruhee, Ruheea Taskin, Sihui Ma, and Katsuhiko Suzuki. "Sulforaphane protects cells against lipopolysaccharide-stimulated inflammation in murine macrophages." Antioxidants 8.12 (2019): 577.
->Talukdar, Jayanta, et al. "COVID-19: Potential of microalgae derived natural astaxanthin as adjunctive supplement in alleviating cytokine storm." Available at SSRN 3579738 (2020).
->Talukdar, Jayanta, et al. "COVID-19: Potential of microalgae derived natural astaxanthin as adjunctive supplement in alleviating cytokine storm." SSRN 3579738 (2020).
->Connors, Jean Marie, and Jerrold H. Levy. "COVID-19 and its implications for thrombosis and anticoagulation." Blood (2020).
->Jose, Ricardo J., and Ari Manuel. "COVID-19 cytokine storm: the interplay between inflammation and coagulation." The Lancet Respiratory Medicine (2020).
->High Fat Intake Leads to Acute Postprandial Exposure to Circulating Endotoxin in Type 2 Diabetic Subjects, Harte et al. Diabetes Care 35:375–382, 2012.
->Ma, Ding, et al. "NLRX1 alleviates lipopolysaccharide-induced apoptosis and inflammation in chondrocytes by suppressing the activation of NF-κB signaling." International immunopharmacology 71 (2019): 7-13.
->Uribarri, Jaime, et al. "Dietary advanced glycation end products and their role in health and disease." Advances in nutrition 6.4 (2015): 461-473.
->European Commission of the European Union (2020) EU Register of nutrition and health claims made on foods. https://ec.europa.eu/food/safety/labelling_nutrition/claims/
register/public/?event=register.home (accessed July 2020).
->Alvarado, Carmen, et al. "Dietary supplementation with antioxidants improves functions and decreases oxidative stress of leukocytes from prematurely aging mice." Nutrition 22.7-8 (2006): 767-777.
->Park, Yikyung, et al. "Dietary fiber intake and mortality in the NIH-AARP diet and health study." Archives of internal medicine 171.12 (2011): 1061-1068.
->Péter S., Eggersdorfer M., Weber P. (2019) Vitamin E Intake and Serum Levels in the General Population: A Global Perspective. In: Weber P., Birringer M., Blumberg J., Eggersdorfer M., Frank J. (eds) Vitamin E in Human Health. Nutrition and Health. Humana Press, Cham.
->Steele, Irena, Daniel Allright, and Roger Deutsch. "A randomized observational analysis examining the correlation between patients’ food sensitivities, micronutrient deficiencies, oxidative stress response and immune redox status." Functional Foods in Health and Disease 10.3 (2020): 143-154.
->Balcerczyk, Aneta, et al. "Enhanced antioxidant capacity and anti-ageing biomarkers after diet micronutrient supplementation." Molecules 19.9 (2014): 14794-14808.
->Dror and Stern. "Micronutrient supplementation in the elderly." Agro Food Industry Hi Tech 15.3 (2004): 30-33.
->Johnson, Ann, and Kimberly H. Porter. "Micronutrient supplementation and infection in institutionalized elders." Nutrition reviews 55.11 (1997): 400-404.
->Girodon, François, et al. "Effect of micronutrient supplementation on infection in institutionalized elderly subjects: a controlled trial." Annals of nutrition and metabolism 41.2 (1997): 98-107.
->High, Kevin P. "Micronutrient supplementation and immune function in the elderly." Clinical infectious diseases 28.4 (1999): 717-722.
->Kononenko, V. V., et al. "The use of the Multi-Tabs vitamin and mineral complex to prevent influenza." Likars' ka sprava 3 (1998): 107-109.
->Sangeetha, Narayanasamy, and S. Premakumari. "Effect of micronutrient supplementation on the nutritional and immune status of school going children with vitamin A deficiency in the urban areas of Chennai District." Journal of Human Ecology 31.1 (2010): 37-46.
->Haryanto, B., et al. "Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality." Vitam. Miner 4 (2015): 1-15.
->Mawson, Anthony R. "Role of Fat-Soluble Vitamins A and D in the Pathogenesis of Influenza: A New Perspective." ISRN Infectious Diseases 2013 (2012).
->Raharusun, Prabowo. "Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study." Available at SSRN 3585561 (2020).
->Grant, William B., et al. "Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths." Nutrients 12.4 (2020): 988.
->Glinsky, Gennadi V. "Genomics-guided tracing of SARS-CoV-2 targets in human cells identifies Vitamin D and Quercetin as candidate medicinal agents for mitigation of the severity of pandemic COVID-19." Chemrxiv.
->Ghavideldarestani, Maryam, Maryam Honardoost, and Mohammad E. Khamseh. "Role of Vitamin D in Pathogenesis and Severity of COVID-19 Infection." (2020). PrePrints.
->Martineau, Adrian R., et al. "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data." bmj 356 (2017): i6583.
->Narayanan, Naveen, and Deepak T. Nair. "Vitamin B12 May Inhibit RNA-Dependent-RNA Polymerase Activity of nsp12 from the COVID-19 Virus." (2020).
->Mikkelsen, Kathleen, and Vasso Apostolopoulos. "Vitamin B12, Folic Acid, and the Immune System." Nutrition and Immunity. Springer, Cham, 2019. 103-114.
->Haryanto, B., et al. "Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality." Vitam. Miner 4 (2015): 1-15.
->Kim, Yejin, et al. "Vitamin C is an essential factor on the anti-viral immune responses through the production of interferon-α/β at the initial stage of influenza A virus (H3N2) infection." Immune network 13.2 (2013): 70-74.
->Vitamin C Deficiency Increases the Lung Pathology of Influenza Virus–Infected Gulo−/− Mice, Wei Li, Nobuyo Maeda, Melinda A. Beck, The Journal of Nutrition, Volume 136, Issue 10, October 2006, Pages 2611–2616.
->Haryanto, B., et al. "Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality." Vitam. Miner 4 (2015): 1-15.
->Péter S., Eggersdorfer M., Weber P. (2019) Vitamin E Intake and Serum Levels in the General Population: A Global Perspective. In: Weber P., Birringer M., Blumberg J., Eggersdorfer M., Frank J. (eds) Vitamin E in Human Health. Nutrition and Health. Humana Press, Cham.
->Han, Sung Nim, et al. "Effect of long-term dietary antioxidant supplementation on influenza virus infection." The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 55.10 (2000): B496-B503.
->Mileva, Milka, and Angel S. Galabov. "Vitamin E and Influenza Virus Infection." Vitamin E in Health and Disease (2018): 67.
->Haryanto, B., et al. "Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality." Vitam. Miner 4 (2015): 1-15.
->Hayek, Michael G., et al. "Vitamin E supplementation decreases lung virus titers in mice infected with influenza." Journal of Infectious Diseases 176.1 (1997): 273-276.
->Wu, Dayong, et al. "Age-associated increase in PGE2 synthesis and COX activity in murine macrophages is reversed by vitamin E." American Journal of Physiology-Cell Physiology 275.3 (1998): C661-C668.
->Meydani, Simin Nikbin, et al. "Vitamin E supplementation and in vivo immune response in healthy elderly subjects: a randomized controlled trial." Jama 277.17 (1997): 1380-1386.
->Lewis, Erin Diane, Simin Nikbin Meydani, and Dayong Wu. "Regulatory role of vitamin E in the immune system and inflammation." IUBMB life 71.4 (2019): 487-494.
->Mileva, Milka, and Angel S. Galabov. "Vitamin E and Influenza Virus Infection." Vitamin E in Health and Disease (2018): 67.
->Lewis, Erin Diane, Simin Nikbin Meydani, and Dayong Wu. "Regulatory role of vitamin E in the immune system and inflammation." IUBMB life 71.4 (2019): 487-494.
->Gay, Raina, et al. "The effect of vitamin E on secondary bacterial infection after influenza infection in young and old mice." Annals of the New York Academy of Sciences 1031.1 (2004): 418-421.
->Hemilä, Harri. "Vitamin E administration may decrease the incidence of pneumonia in elderly males." Clinical interventions in aging 11 (2016): 1379.
->Han, S. N., et al. "Vitamin E supplementation increases T helper 1 cytokine production in old mice infected with influenza virus." Immunology 100.4 (2000): 487-493.
->Gay, Raina, and Simin Nikbin Meydani. "The effects of vitamin E, vitamin B6, and vitamin B12 on immune function." Nutrition in Clinical Care 4.4 (2001): 188-198.
->Haryanto, B., et al. "Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality." Vitam. Miner 4 (2015): 1-15.
->Ha, C., L. T. Miller, and N. I. Kerkvliet. "The effect of vitamin B6 deficiency on cytotoxic immune responses of T cells, antibodies, and natural killer cells, and phagocytosis by macrophages." Cellular immunology 85.2 (1984): 318-329.
->Haryanto, B., et al. "Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality." Vitam. Miner 4 (2015): 1-15.
->Shi, Qiujun, et al. "Selenium deficiency increases the pathology of an influenza virus infection." The FASEB Journal express article 10.1096/fj.00-0721fje. 2001.
->Fraker, Pamela J., et al. "The dynamic link between the integrity of the immune system and zinc status." The Journal of Nutrition 130.5 (2000): 1399S-1406S.
->Duchateau, Jean, et al. "Beneficial effects of oral zinc supplementation on the immune response of old people." The American journal of medicine 70.5 (1981): 1001-1004.
->Haryanto, B., et al. "Multivitamin supplementation supports immune function and ameliorates conditions triggered by reduced air quality." Vitam. Miner 4 (2015): 1-15.
->Razzaque, Mohammed. "COVID-19 Pandemic: Can Maintaining Optimal Zinc Balance Enhance Host Resistance?." (2020).
->Read, Scott A., et al. "The role of zinc in antiviral immunity." Advances in Nutrition 10.4 (2019): 696-710.
->Cakman, Irem, HOLGER KIRCHNER, and LOTHAR RINK. "Zinc supplementation reconstitutes the production of interferon-α by leukocytes from elderly persons." Journal of interferon & cytokine research 17.8 (1997): 469-472.
->Heidary, Fatemeh, Mehran Varnaseri, and Reza Gharebaghi. "The Potential Use of Persian Herbal Medicines Against COVID-19 Through Angiotensin-Converting Enzyme 2." Archives of Clinical Infectious Diseases 15.2020.
->Khan, Mohammad Faheem, et al. "Identification of Dietary Molecules as Therapeutic Agents to Combat COVID-19 Using Molecular Docking Studies." (2020).
->Adem, Sevki, et al. "Identification of potent COVID-19 main protease (Mpro) inhibitors from natural polyphenols: An in silico strategy unveils a hope against CORONA." (2020).PrePrint.
->Yonesi, Mahdi, and Alireza Rezazadeh. "Plants as a Prospective Source of Natural Anti-viral Compounds and Oral Vaccines Against COVID-19 Coronavirus." (2020).
->G. Hoever et al., "Antiviral Activity of Glycyrrhizic Acid Derivatives against SARS-Coronavirus," Journal of medicinal chemistry, vol. 48, no. 4, pp. 1256-1259, 2005.
->J. Pu, L. He, S. Wu, P. Zhang, and X. Huang, "Anti-virus research of triterpenoids in licorice,"Bing du xue bao, Chinese journal of virology, vol. 29, no. 6, pp. 673-679, 2013.
->Yonesi, Mahdi, and Alireza Rezazadeh. "Plants as a Prospective Source of Natural Anti-viral Compounds and Oral Vaccines Against COVID-19 Coronavirus." (2020).
->H. Liu et al., "Scutellaria baicalensis extract and baicalein inhibit replication of SARS-CoV-2 and its 3C-like protease in vitro," bioRxiv, p. 2020.04.10.035824, 2020, doi:10.1101/2020.04.10.035824.
->Adem, Sevki, et al. "Identification of potent COVID-19 main protease (Mpro) inhibitors from natural polyphenols: An in silico strategy unveils a hope against CORONA." (2020).PrePrint.
->Glinsky, Gennadi V. "Genomics-guided tracing of SARS-CoV-2 targets in human cells identifies Vitamin D and Quercetin as candidate medicinal agents for mitigation of the severity of pandemic COVID-19." 2020, Chemrxiv.
->Glinsky, Gennadi V. "Genomics-guided tracing of SARS-CoV-2 targets in human cells identifies Vitamin D and Quercetin as candidate medicinal agents for mitigation of the severity of pandemic COVID-19." 2020, Chemrxiv.
->Omar, Sekiou, et al. "In-Silico Identification of Potent Inhibitors of COVID-19 Main Protease (Mpro) and Angiotensin Converting Enzyme 2 (ACE2) from Natural Products: Quercetin, Hispidulin, and Cirsimaritin Exhibited Better Potential Inhibition than Hydroxy-Chloroquine Against COVID-19 Main Protease Active Site and ACE2." (2020).
->Wahedi, Hussain Mustatab, Sajjad Ahmad, and Sumra Wajid Abbasi. "Stilbene-based Natural Compounds as Promising Drug Candidates against COVID-19." Journal of Biomolecular Structure and Dynamics just-accepted (2020): 1-16.
->Pendyala, Brahmaiah, and Ankit Patras. "In silico Screening of Food Bioactive Compounds to Predict Potential Inhibitors of COVID-19 Main protease (Mpro) and RNA-dependent RNA polymerase (RdRp)." (2020).
->Pendyala, Brahmaiah, and Ankit Patras. "In silico Screening of Food Bioactive Compounds to Predict Potential Inhibitors of COVID-19 Main protease (Mpro) and RNA-dependent RNA polymerase (RdRp)." (2020).
->Khaerunnisa, Siti, et al. "Potential Inhibitor of COVID-19 Main Protease (Mpro) From Several Medicinal Plant Compounds by Molecular Docking Study." Prepr. doi10. 20944/preprints202003. 0226. v1 (2020): 1-14.
->Yonesi, Mahdi, and Alireza Rezazadeh. "Plants as a Prospective Source of Natural Anti-viral Compounds and Oral Vaccines Against COVID-19 Coronavirus." (2020).
->Adem, Sevki, et al. "Identification of potent COVID-19 main protease (Mpro) inhibitors from natural polyphenols: An in silico strategy unveils a hope against CORONA." (2020). PrePrint.
->S. Jo, S. Kim, D. H. Shin, and M.-S. Kim, "Inhibition of SARS-CoV 3CL protease by flavonoids," Journal of Enzyme Inhibition and Medicinal Chemistry, vol. 35, no. 1, pp. 145-151, 2020/01/01 2020, doi: 10.1080/14756366.2019.1690480.
->Omar, Sekiou, et al. "In-Silico Identification of Potent Inhibitors of COVID-19 Main Protease (Mpro) and Angiotensin Converting Enzyme 2 (ACE2) from Natural Products: Quercetin, Hispidulin, and Cirsimaritin Exhibited Better Potential Inhibition than Hydroxy-Chloroquine Against COVID-19 Main Protease Active Site and ACE2." (2020).
->Srivastava, Ambrish Kumar, Abhishek Kumar, and Neeraj Misra. "On the Inhibition of COVID-19 Protease by Indian Herbal Plants: An In Silico Investigation." arXiv preprint arXiv:2004.03411 (2020).
->Adem, Sevki, et al. "Identification of potent COVID-19 main protease (Mpro) inhibitors from natural polyphenols: An in silico strategy unveils a hope against CORONA." (2020).PrePrint.
->Adem, Sevki, et al. "Identification of potent COVID-19 main protease (Mpro) inhibitors from natural polyphenols: An in silico strategy unveils a hope against CORONA." (2020).PrePrint.
->C.W. Lin et al., "Anti-SARS coronavirus 3C-like protease effects of Isatis indigotica root and plant-derived phenolic compounds," Antiviral Research, vol. 68, no. 1, pp. 36-42, 2005/10/01/2005.
->Adem, Sevki, et al. "Identification of potent COVID-19 main protease (Mpro) inhibitors from natural polyphenols: An in silico strategy unveils a hope against CORONA." (2020).PrePrint.
->Linani, Abderahmane, Khedidja Benarous, and Mohamed Yousfi. "Novel Structural Mechanism of Glutathione as a potential peptide inhibitor to the main protease (Mpro): CoviD-19 treatment, Molecular docking and SAR study." (2020). ChemRxiv.
->Spearow, Jimmy L., and Linda Copeland. "Improving Therapeutics for COVID-19 with Glutathione-boosting Treatments that Improve Immune Responses and Reduce the Severity of Viral Infections." (2020).
->Naik, Suresh Ramnath, Vishnu Namdeorao Thakare, and Falguni P. Joshi. "Functional foods and herbs as potential immunoadjuvants and medicines in maintaining healthy immune system: A commentary." Journal of Complementary and Integrative Medicine 7.1 (2010).
->Vimalanathan, Selvarani, et al. "Prevention of influenza virus induced bacterial superinfection by standardized Echinacea purpurea, via regulation of surface receptor expression in human bronchial epithelial cells." Virus research 233 (2017): 51-59.
->Naik, Suresh Ramnath, Vishnu Namdeorao Thakare, and Falguni P. Joshi. "Functional foods and herbs as potential immunoadjuvants and medicines in maintaining healthy immune system: A commentary." Journal of Complementary and Integrative Medicine 7.1 (2010).
->Mallard, Brody, et al. "Synergistic immuno-modulatory activity in human macrophages of a medicinal mushroom formulation consisting of Reishi, Shiitake and Maitake." PloS one 14.11 (2019): e0224740-e0224740.
->Turmagambetova, Aizhan Sabirzhanovna, et al. "New functionally-enhanced soy proteins as food ingredients with anti-viral activity." VirusDisease 26.3 (2015): 123-132.
->Naik, Suresh Ramnath, Vishnu Namdeorao Thakare, and Falguni P. Joshi. "Functional foods and herbs as potential immunoadjuvants and medicines in maintaining healthy immune system: A commentary." Journal of Complementary and Integrative Medicine 7.1 (2010).
->S Bouchentouf, N Missoum, " Identification of Compounds from Nigella Sativa as New Potential Inhibitors of 2019 Novel Coronasvirus (Covid-19): Molecular Docking Study." ChemRxiv (2020).
->Kim, Hyemin, et al. "Red ginseng and vitamin C increase immune cell activity and decrease lung inflammation induced by influenza A virus/H1N1 infection." Journal of Pharmacy and Pharmacology 68.3 (2016): 406-420
->Shin, Kun Kuk, et al. "Korean Red Ginseng Plays An Anti-Aging Role by Modulating Expression of Aging-Related Genes and Immune Cell Subsets." Molecules 25.7 (2020): 1492.
->Naik, Suresh Ramnath, Vishnu Namdeorao Thakare, and Falguni P. Joshi. "Functional foods and herbs as potential immunoadjuvants and medicines in maintaining healthy immune system: A commentary." Journal of Complementary and Integrative Medicine 7.1 (2010).
->Hwang, Bang Yeon, et al. "Antimicrobial constituents from goldenseal (the Rhizomes of Hydrastis canadensis) against selected oral pathogens." Planta medica 69.07 (2003): 623-627.
->Naik, Suresh Ramnath, Vishnu Namdeorao Thakare, and Falguni P. Joshi. "Functional foods and herbs as potential immunoadjuvants and medicines in maintaining healthy immune system: A commentary." Journal of Complementary and Integrative Medicine 7.1 (2010).
->Liang, Yuxi, et al. "Astragalus Membranaceus Treatment Protects Raw264. 7 Cells from Influenza Virus by Regulating G1 Phase and the TLR3-Mediated Signaling Pathway." Evidence-Based Complementary and Alternative Medicine 2019 (2019).
->Naik, Suresh Ramnath, Vishnu Namdeorao Thakare, and Falguni P. Joshi. "Functional foods and herbs as potential immunoadjuvants and medicines in maintaining healthy immune system: A commentary." Journal of Complementary and Integrative Medicine 7.1 (2010).
->Lai, Yanni, et al. "3D-quantitative structure–activity relationship and antiviral effects of curcumin derivatives as potent inhibitors of influenza H1N1 neuraminidase." Archives of Pharmacal Research (2020): 1.
->Bidian, Cristina, et al. "Quercetin and curcumin effects in experimental pleural inflammation." Medicine and Pharmacy Reports (2020).
->Naik, Suresh Ramnath, Vishnu Namdeorao Thakare, and Falguni P. Joshi. "Functional foods and herbs as potential immunoadjuvants and medicines in maintaining healthy immune system: A commentary." Journal of Complementary and Integrative Medicine 7.1 (2010).
->Mehrbod, P., E. Amini, and M. Tavassoti-Kheiri. "Antiviral activity of garlic extract on influenza virus." Iranian journal of Virology 3.1 (2009): 19-23.
->Nantz, Meri P., et al. "Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: a randomized, double-blind, placebo-controlled nutrition intervention." Clinical Nutrition 31.3 (2012): 337-344.
->Zhang, D., et al. "Molecular Basis for Treating COVID-19 with Official Chinese Herbal Formula LCTE." (2020). Preprints.
->Zhang, D., et al. "Molecular Basis for Treating COVID-19 with Official Chinese Herbal Formula LCTE." (2020). Preprints.
->Runfeng, Li, et al. "Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2)." Pharmacological research (2020): 104761.
